DIETARY SALT and BP: Is there a sweet spot?
For decades salt (i.e. sodium chloride) has been caught up in an interminable debate about the relationship between diet and health. The reason for all the popular focus on dietary salt intake is its purported association with high blood pressure.

High blood pressure (hypertension), causes early death from stroke and heart disease and it’s been described as Australia’s biggest killer.
According to the Heart Foundation more than 6 million Australians (34% or 1 in 3) have high blood pressure (BP) — as defined by a systolic BP equal to or greater than 140 mmHg and a diastolic BP equal to or greater than 90 mmHg. Half of those people with hypertension don’t even know they have it.
In most people with hypertension (85%-95%) there is no specific identifiable cause of their high blood pressure,(such as a tumour of the adrenal gland) — they have what is known as “ essential” or primary hypertension. Genes are suspected of playing a role in up to 60% of people with hypertension and it’s interesting that all of the genes identified so far as having a link with hypertension are associated with mechanisms of sodium transport.
So that in many people with hypertension, the way in which the body handles salt is obviously playing a role. However, the question is “How much does the level of dietary salt intake influence those mechanisms ?”
If a high salt intake can be incriminated in causing high blood pressure, then we, and our public health system should be doing everything possible to curb that intake.
In this article we’re going to examine that link between dietary salt and blood pressure, as revealed in a recent comprehensive meta-analysis of the current data. This study looked at all the available randomised trials carried out to date which have compared the effects of a low-sodium diet versus a high-sodium diet on BP.
Some of the conclusions may come as a bit of a surprise.
But first, some background.
SALT OF THE EARTH — ITS PLACE IN THE HUMAN HISTORY
Sodium is necessary for our survival and yet we are unable to make it ourselves.
Over much of the 2 million years or so of human evolution, sodium, in its most common form as sodium chloride, or salt, was rare and inaccessible. It is only in the past few hundred years or so that is has become easily procurable.
Salt’s scarcity created intense evolutionary pressure for the selection of genes which coded for salt-conserving physiologic processes. The most important of these is the renin-angiotensin-aldosterone system (RAAS), which we will come back to a little later in the story.
The history of salt and its role in the march of human civilisation is truly fascinating (ref: “Salt : A World History” by Mark Kurlansky; 2002; Thorndike Press). The discovery of its preservative property, which allowed food to be stored before refrigeration, was momentous and provided the means by which man was able to transition from a hunter- gatherer to a farmer.
Salt consequently became a major economic commodity, sparking border disputes and wars. Roman soldiers were partly paid in salt (Latin salarium )and it’s from this we get the word ‘soldier’– sal dare, meaning to give salt — and the word ‘salary’.
Salt was often heavily taxed, becoming the principal source of State revenue for many governments around the world. Like any onerous taxes, they often caused much resentment among the populace. Indeed, the French gabelle salt tax may have helped incite the French Revolution and salt taxes provided the spark for Ghandi’s independence movement and his defiant Salt March, which was pivotal to the ending of British rule in India.
The availability of cheap, purified table salt is a relatively recent development, coming only after modern geology helped identify abundant salt deposits accessible to mining throughout the world and the technology was developed to permit its extraction in large quantities. Now salt is so cheap that more than 50% of salt mined in America is used for de-icing roads in winter ; only 8 percent of salt production is for food.
HOW IS SALT BALANCE IN THE BODY REGULATED?
Homo sapien’s distant ancestors evolved from life forms that originated in the sea. To free themselves from this salty marine environment and to transition to life on land, these life forms had to develop the ability to effectively carry the sea within them — creating an internal salty fluid “milieu interior”, which comprises two compartments in the body — the fluid inside the cells ( intracellular fluid, or ICF) and the fluid bathing the cells, (extracellular fluid, or ECF).
Indeed, water makes up approximately 60% of our total body weight, two-thirds of which is located within the ICF compartment and one-third in the ECF.
From the point of view of salt regulation, the focus is on the ECF compartment because this is where 98% of total-body sodium is contained in young, healthy humans. The volume and salt composition of the ECF is maintained in a steady state by a complex interplay of age-old neurophysiological and hormonal control mechanisms designed to balance water and salt intake with their matched excretion by the kidneys — part of the whole body system of stabilising the milieu interior, known as homeostasis.
For those of you interested in learning about these homeostatic control mechanisms in more detail, the following section will be of interest but it can probably be skipped over by the casual reader — but you may miss some interesting facts about ACE!
RENIN-ANGIOTENSIN-ALDOSTERONE SYSTEM
Principal among these homeostatic control mechanisms is the aforementioned renin-angiotensin-aldosterone system, or RAAS.
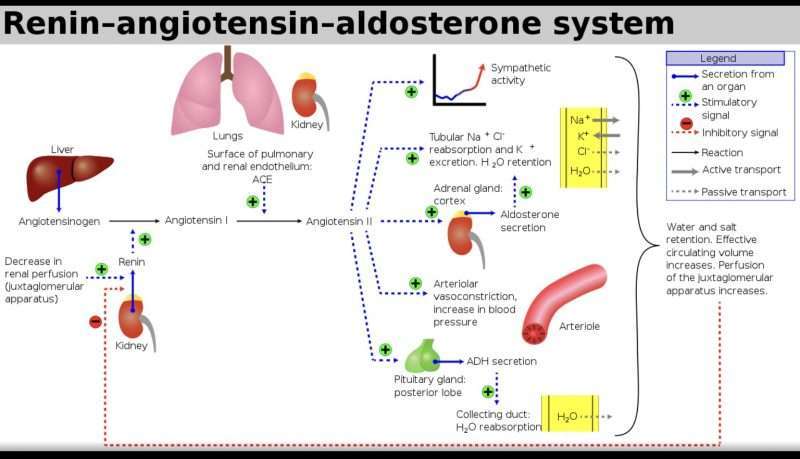
Even small decreases in ECF volume produce decrements in blood volume and blood pressure. These changes are detected by exquisitely sensitive, specialised cells in the kidney, triggering them to secrete an enzyme, called renin, into the blood.
Renin acts on a circulating protein which is made in the liver, called angiotensinogen, cleaving this substance into angiotensin I which is, in turn, converted into angiotensin II by contact with an enzyme called Angiotensin Converting Enzyme, or simply, ACE, located principally in the lungs. Angiotensin II stimulates the release of a hormone called aldosterone made in the adrenal glands.
The biological action of aldosterone is to increase the retention of sodium ( in exchange for potassium) and water by the kidney. It acts by binding to a receptor in the cytoplasm of the renal tubular cells. The activated receptor then stimulates the production of ion channels in the renal tubular cells, thereby increasing sodium reabsorption into the blood and increasing potassium excretion into the urine.
Aldosterone therefore affects blood pressure by increasing or decreasing the sodium content and volume of the extracellular fluid.
ACE – SNAKES, ANTIHYPERTENSIVES and COVID
The Discovery of ACE-Inhibitors
In the 1970’s the pharmaceutical industry targeted ACE for the treatment of hypertension by developing drugs that could inhibit ACE . The aim was to block aldosterone production (by blocking the conversion of angiotensin I to angiotensinII), thereby increasing the excretion of sodium by the kidneys and causing a contraction in ECF volume to lower blood pressure.
This effort came about quite serendipitously by the discovery in the research lab of a consultant to the pharmaceutical giant, E.R Squibb and Sons, that the venom from a poisonous Brazilian viper contained peptides which inhibited ACE. A bite from this snake causes an instant drop in blood pressure in its prey, making escape impossible.
This first peptide extract from the snake venom could not be taken by mouth, so further studies were carried out in the lab to synthesise a similar peptide which was orally active (thus sparing the snakes from further exploitation!)
This medication was called Captopril (Trade name Capo- ten), and was Sqibb’s first billion dollar drug. It opened a new approach to the treatment of hypertension and it is now among the most common class of hypertensive medications.
Now, what about that suggested link between ACE- inhibitors and COVID-19?
In early part of 2020 when the COVID -19 epidemic was just getting underway, statements appeared in the press suggesting that people taking ACE-inhibitors for blood pressure control could be at higher risk of coronavirus infection and at higher risk of severe or fatal coronavirus symptoms.
The suggested link was based on the observation that ACE inhibitors increase levels of the ACE enzyme in the body, which of all things happens to be the very same enzyme that the coronavirus uses to infect the body, binding to it in the lungs with its spike protein.
The improbable juxtaposition of these phenomena seemed like the worst-case scenario imaginable — as if it were dreamed up in some sort of twisted, dystopian world.
For the millions of people on ACE inhibitor medication, the prospect was frightening. The issue had to be addressed urgently!
In May 2020, the New England Journal of Medicine responded by publishing three large observational studies from around the globe, involving thousands of patients who had contracted COVID-19, which specifically examined the question as whether ACE inhibitors were indeed harmful.
Their message was consistent and clear — none of the studies revealed any higher risk of infection or of more serious disease, with the continued use of ACE inhibitors.
Doctors and their patients breathed a huge sigh of relief.
NOW FOR THE MEAT OF THE MATTER – IS DIETARY SALT HARMFUL?
No-one questions the body’s need for salt and and it is also generally accepted that there is a link between high BP, cardiovascular disease and the consumption of too much salt.
But how much is too much ? And, can you become unhealthy from eating too little salt ?
A couple of years ago I would say that the court of public health opinion was swinging decidedly toward the viewpoint that we were all eating too much salt.
Efforts were underway to increase public awareness of the perceived harmful effects of salt on health and a worldwide campaign, sponsored by the WHO, was being promoted internationally to reduce dietary salt intake to less than 5 g per day.
Recently, however, such efforts have come under question.
The reason has been the publication of new information from a comprehensive, large scale re-evaluation of collected global data looking at contemporary levels of dietary salt intake and at the limited health results that can be achieved by reducing salt consumption.
THE COCHRANE META-ANALYSIS OF 2020
When you’re trying to evaluate the effects of a therapeutic intervention in public health, the best evidence is obtained from what is called a meta-analysis.
Such an analysis combines the results of all the available randomised trials which have been undertaken in order to obtain the most reliable estimates of the size of those effects.
By improving the precision and accuracy of those estimates, a meta-analysis increases the statistical power to detect or reject an effect.

In December 2020 the Cochrane Collaboration* published such a meta-analysis of all the available randomised trials from around the world looking at the effects of a low- sodium diet versus a high-sodium diet on BP.
In total, 195 studies, involving 12,296 individuals were examined. The mean salt intake for the populations studied was reduced from approximately 11 grams/day to 4 grams/ day.
I would stress that only randomised controlled trials were included and salt intake was measured by the accepted gold standard technique of 24-hr urinary excretion. The grade of evidence for the meta-analysis was therefore considered to be high.
The Results of Switching to a Lower Salt Intake :
• In people with normal BP : the mean BP decreased by
0.4 mmHg ( 0.3%)
• In people with high blood pressure : the mean BP decreased 4mmHg (3%j.
• The effect on various hormones listed below were similar in both groups : all were increased by the percentages shown :
Renin 55%
Aldosterone 127%
Adrenaline 14%
Noradrenaline 27%.
It was concluded from these studies that:
• In people with a normal BP, dietary salt reduction has no apparent benefit.
• In people with hypertension, it may cause a slight reduction in BP.
• The hormonal changes observed might provide a possible explanation for such a slight change in BP —namely, the compensatory activation of the RAAS system. This is indicated by the substantial increases in renin and aldosterone levels. The significant rise in noradrenaline and adrenaline levels may also contribute to this counter- regulation by causing vasoconstriction and some increase in heart rate — changes which, incidentally, could be of some concern to cardiovascular health.
So, the upshot is, that while it might be reasonable to consider reducing dietary salt intake as a supplementary treatment for individuals with hypertension, the case for doing so on a population-wide basis is more contentious.
It also seems apparent from the data that there isn’t much wrong with our present average level of salt intake.
According to the Cochrane meta-analysis, which looked at the baselines levels of salt intake in a great many apparently healthy populations around the world — the average intake is approximately 9 grams/day.— a far cry from the WHO recommended intake of 5 grams/day.
The Institute of Medicine defines an adequate nutritional intake as “ the appropriate intake found in apparently healthy populations.”

This is what 8 grams of salt looks like
As the authors of the Cochrane study suggest, it may be appropriate to accept the present usual sodium intake of 9 grams/day in apparently healthy populations as the optimal intake for the general population. It might even be necessary, they also suggested, to revise the present process of establishing national dietary guidelines, especially when one considers the concern, expressed by some experts, that reducing salt intake below 6grams/day might even be harmful.
If one looks at the relationship between levels of salt intake and mortality, several observational population studies have suggested that this takes the form of a U-shaped curve — with levels below 6 grams/day, and above 12 grams/day, both being associated with increased mortality.
So, 9 grams/day sounds just about right — is this the sweet spot?
WHAT IS THE TAKEAWAY MESSAGE?
I think it is evident that data gleaned from the most up-to- date and reliable meta-analysis, does not support the notion that dietary salt reduction has any beneficial effects on people with normal BP.
People who have diagnosed hypertension may derive some benefit, in terms of BP control, from reducing their salt intake, but it is not very impressive. Reducing salt intake in these individuals is perhaps best achieved by reducing the consumption of processed foods (which are typically high in salt content). They should also consider limiting the amount of salt which is added when preparing food and when sprinkling it on meals.
A FINAL COMMENT
There is some evidence to suggest that it would be better for all of us if we used a potassium-containing salt substitute (75% NaCl, 25% potassium chloride) rather than common table salt (100% NaCl). A recent large, randomised trial showed that persons who consumed the substitute salt, as opposed to those who used typical salt, not only had lower blood pressure but also had lower rates of stroke, major cardiovascular events, and death.
*Footnote : The Cochrane Collaboration is an international, not-for-profit organisation that promotes, supports and disseminates systematic reviews and meta-analyses of interventions in the healthcare field and is highly trusted by health care professionals.
* Words by Dr Tony Edis MD
In case you missed Dr Edis MD’s previous articles here they are –
#1 addressed the Intermittent Fasting trend
#2 dealt with the Food Guide Pyramid and dietary fat.
#3 discussed the ‘Lowdown’ on cholesterol and statins
#4 explained what to do when someone has a heart attack
#5 discusses the ‘miracle molecule’ Nitric Oxide
PLEASE HELP US TO GROW FREMANTLE SHIPPING NEWS
FSN is a reader-supported, volunteer-assisted online magazine all about Fremantle. Thanks for helping to keep FSN keeping on!
** Don’t forget to SUBSCRIBE to receive your free copy of The Weekly Edition of the Shipping News each Friday!






