How does Omicron compare with Delta? Here’s what we know about infectiousness, symptoms, severity and vaccine protection
Since Omicron was detected in South Africa in late November, the SARS-CoV-2 variant has spread to more than 165 countries and is now the dominant strain.
Omicron has more mutations than other strains: 72 in total, the most concerning of which make the virus more transmissible and better able to evade the immune system and vaccines.
So how does Omicron differ to Delta in infectiousness, symptoms, severity and vaccine protection.
How contagious is it?
The basic reproduction number (R0) is one gauge of the infectiousness of a virus. It tells you how many susceptible people a single infected person will themselves go on to infect.
Danish researchers estimate the effective reproduction number of Omicron is 3.19 times more than that of Delta, which had an average R0 of 5 (ranging from 3.2 to 8).
Similarly, Japanese research concludes Omicron is 4.2 times more transmissible than Delta early on.
So, in a fully susceptible (unvaccinated and uninfected) population, one person with Delta would, on average, infect five other people, while one person with Omicron could transmit the virus to about 20 others.
This makes Omicron one of the most infectious agents known.

Another practical indicator of a virus’s infectiousness is how easily it spreads within households. This is known as the secondary attack rate.
Studies from various countries have consistently shown Omicron has a higher secondary attack rate in households than Delta. In a household with Omicron, householders have a 14-50% chance of getting infected.
Why is Omicron more infectious?
Omicron’s varied mutations allow it to evade the immunity generated by both previous infections and vaccination.
Studies have also shown Omicron infects and multiplies in the upper airways 70 times faster than Delta.
There also seems to be more asymptomatic infections with Omicron. This probably facilitates transmission, as people don’t realise they’re infected and will move around normally.
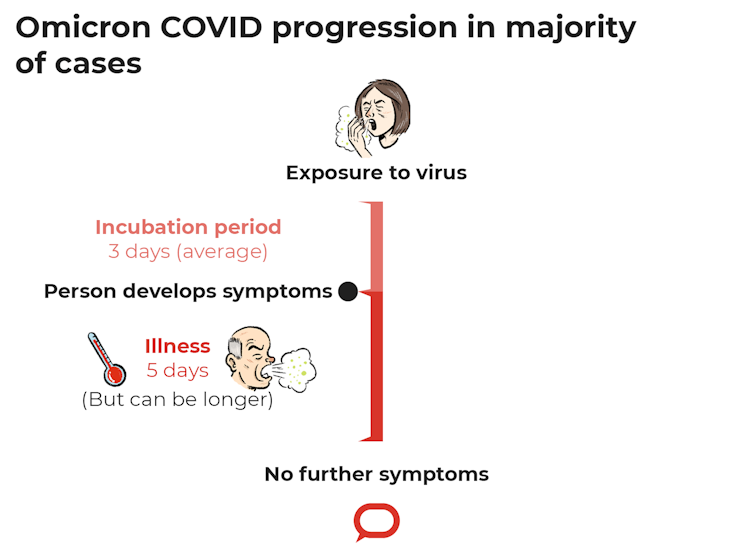
How long does it take to become sick?
The incubation period of Omicron – the period from being infected to getting symptoms – is around three days, with the person often becoming infectious a day or two before symptoms emerge.
This is shorter than with Delta and earlier variants.
The average duration of illness is shorter with Omicron than Delta: five days compared to six.
With new isolation rules implemented during the Omicron wave, seven days after testing positive to COVID, those who are symptom-free will no longer have to isolate.
CC BY-ND
What are the symptoms?
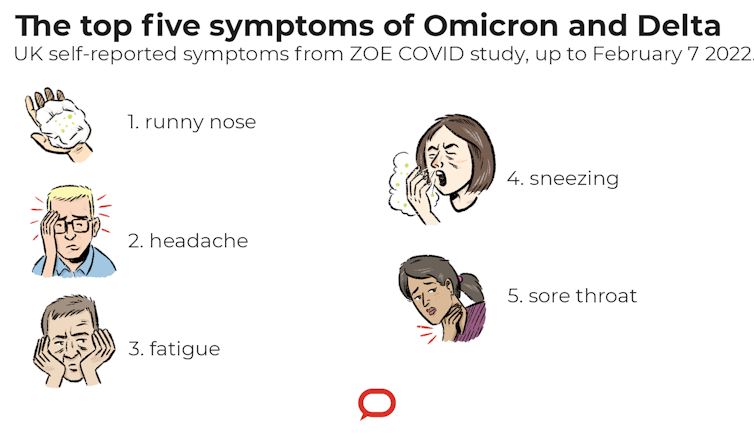
The five most common symptoms of Delta and Omicron are:
- runny nose
- headache
- fatigue
- sneezing
- sore throat.
Compared with Delta, Omicron is more likely to cause a sore throat and less likely to be associated with the loss of taste or smell.
CC BY-ND
In children, Omicron may be more likely to cause croup, which leads to a distinctive barking cough. Croup is associated with other viruses, but Omicron’s ability to infect the upper airways so efficiently may allow it to cause croup more than previous COVID variants.
Is it less severe?
Yes, Omicron causes less severe disease than Delta. Part of this may be due to Omicron being less able to infect lungs as it does the upper airways.
The risk of hospitalisation and ICU admissions from Omicron are 40-80% lower than with Delta.
The risk of death is about 60% less with Omicron than with Delta.
Yet despite the reduced severity, this wave of Omicron has been associated with higher rates of hospitalisations in many countries because of the sheer numbers of those infected.
The only silver lining has been how the Omicron wave peaked within a few weeks in numerous countries, with hospitalisation and daily case numbers quickly coming down.
Can you be reinfected with COVID?
Yes, people who have previously had COVID from earlier variants are at risk of getting infected with Omicron, particularly in regions with low vaccination rates.
Analysis of 116,683 cases early in the UK’s Omicron wave found 9.5% of Omicron cases were reinfections.
It’s too early to know the risk of a person previously infected with Omicron getting Omicron again.
How effective are two doses of vaccine?
After 20 weeks, two doses of either mRNA vaccine (Pfizer or Moderna), reduced the risk of infection with Omicron by only around 10%.
By the same point in time, two doses of AstraZeneca essentially provide no protection against infection with Omicron.
However, two doses of vaccine still prevent severe disease, with a vaccine effectiveness against hospitalisation of up to 35% six months later. This is less than half as effective as the protection offered against hospitalisation with Delta.
How effective are three doses of vaccine?
A booster dose of vaccine improves your protection against Omicron. Vaccine effectiveness against hospitalisation is 83% ten or more weeks after the booster.
Protection against symptomatic disease increases too. Vaccine effectiveness is 65-75% two to four weeks after the booster, reducing to 45-50% ten weeks after the booster.
Pfizer and Moderna have also developed an Omicron-specific vaccine which they are about to test in clinical trials and could be available in the second half of 2022. ![]()
Sanjaya Senanayake, Associate Professor of Medicine, Infectious Diseases Physician, Australian National University
This article is republished from The Conversation under a Creative Commons license. Read the original article.
PLEASE HELP US TO GROW FREMANTLE SHIPPING NEWS
FSN is a reader-supported, volunteer-assisted online magazine all about Fremantle. Thanks for helping to keep FSN keeping on!
**** Don’t forget to SUBSCRIBE to receive your free copy of The Weekly Edition of the Shipping News each Friday!